The Link Between HIV and Cervical Cancer: What You Need to Know
Introduction
Cervical cancer is a prominent health concern as it stands as the second leading cause of death among women. Unfortunately, every woman aged 15 and older is at risk of developing this disease [1]. Various factors contribute to the development of cancer, but people with co-infection with HIV are at greater risk of developing cervical cancer. As a part of the cervical cancer awareness initiative, we aim to delve deeper into the link between HIV and cervical cancer, highlighting important insights that you need to know.
Prevalence of cervical cancer around the world
As per Globocan data, in 2020, globally, 604100 new cases and 341831 deaths of cervical cancer were observed. Though a declining trend of cervical cancer was observed by 39.7% from 1990 to 2016, cervical cancer remained the second leading cause of death in India and 4th most common form of cancer among women worldwide [2].
As per recent data on HPV-related cancer, India alone accounts for 123907 cervical cancer cases every year, and 77348 people die from the disease [3].
What is HIV?
Human immunodeficiency virus (HIV) is a virus that targets and attacks the body’s immune cells (CD4 cells), leading to the continuous replication and destruction of the body’s immunity. The human body weakens over time, leading to the final stage of acquired immunodeficiency syndrome (AIDS). This condition can be transmitted through sexual intercourse or by sharing injections.
Signs to recognize HIV:
- Swollen lymph nodes
- Fever
- Fatigue
- Muscle aches
- Rash
- Chills
- Sore throat
- Mouth ulcers
- Night sweats
What is HPV?
Human papillomavirus (HPV) infection is commonly transmitted through skin-to-skin contact or sexual intercourse. While symptoms may not manifest immediately, the infection often results in the formation of warts, and certain types of HPV infections have the potential to progress to cancer.
It’s important to note that whether symptoms are present or not, the virus can be transmitted from person to person. The strains of the human papilloma virus that cause warts are different from those that can lead to cancer.
Signs to recognize HPV:
Though symptoms may appear immediately, some strains cause warts and some can cause cancer.
- Genital warts
- Common warts
- Plantar warts
- Flat warts
How does HPV lead to cervical cancer?
When a person is first infected with HPV, it does not immediately lead to cancer. However, over time, individuals with weakened immune systems may harbor high-risk strains of the virus, which can then proliferate uncontrollably, increasing the risk of developing cervical cancer.
Link Between HIV and HPV in Causing Cervical Cancer
Scientifically, there is no link between HIV and HPV. But various studies show that people with HIV are more vulnerable to HPV infection because the presence of HIV weakens the immune system, which makes it harder for the body to clear HPV infection on its own. Due to this, the HPV infection persists and multiplies abnormally as pre-cancer cells called cervical intraepithelial neoplasia (CIN). These cells, when left untreated, can lead to cervical cancer.
Risk factors for cervical cancer:
Let’s check out the risk factors that increase the risk of getting cervical cancer:
- Multiple sexual partners
- Early sexual activity
- Use of contraceptive pills
- Other sexually transmitted infections (STIs)
- A weakened immune system
- Smoking
Prevention
To avoid HPV-related cancers from developing, the Centers for Disease Control and Prevention (CDC) recommends an FDA-approved vaccine for all pre-teens around ages 11–12 and everyone through age 26 [4].
Practice safe sex using a condom, though it does not protect completely against HPV, it can reduce the transmission of viruses [5].
Global Strategy to Eliminate Cervical Cancer
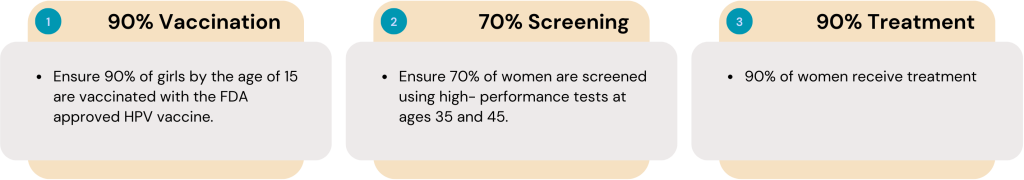
Cervical cancer has the greater potential to be preventable and treatable when it is diagnosed early. The WHO calls for action to eliminate cancer by 2030 in all the countries with a global strategy of 90–70–90 targets and to maintain an incidence rate of below 4 per 100 000 women [6].
Why are regular cervical cancer screenings important?
Health experts strongly advise regular screenings for cervical cancer. Early diagnosis increases the chances of successful treatment and reduces the risk of death associated with cervical cancer.
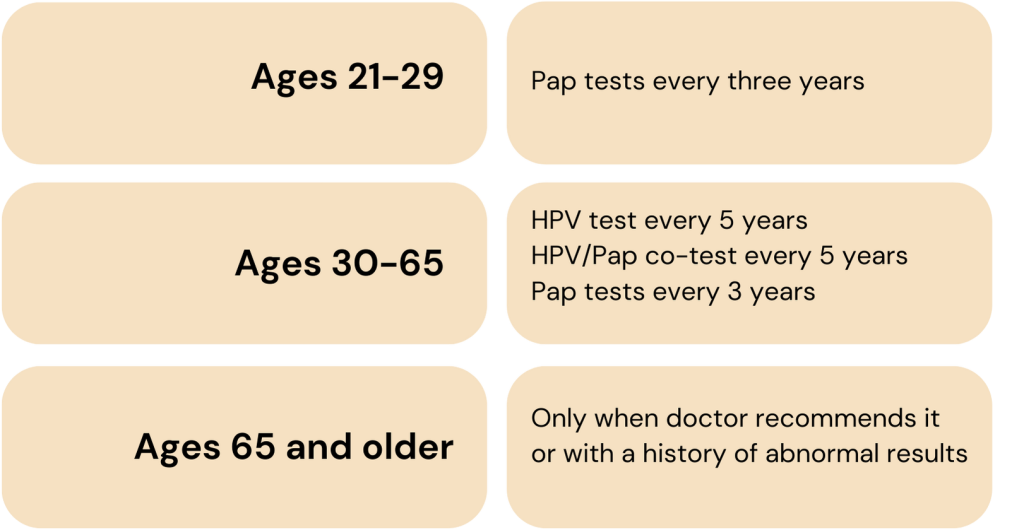
Screenings vary based on age and health history [7]:
What does Yoda diagnostics offer?
Yoda Diagnostics offers a cervical cancer screening package including LBC pap smear tests and HPV DNA tests, commonly termed as co-testing. This is recommended, especially for women aged 30-65 years, to be conducted together, where a pap smear helps assess changes in the cells of the cervix and an HPV DNA test then helps to see whether these changes have occurred due to the presence of high-risk HPV.
Thus, this cervical cancer screening package enables us to detect cervical cancer in its early stages, giving our patients the best chance for successful treatment and recovery.
Final thoughts
Cervical cancer, a prevalent health concern globally, persists as a formidable challenge, being the second leading cause of death among women. As mentioned already, the unfortunate reality is that every woman aged 15 and older is at risk.
Through continued education and proactive healthcare measures via timely diagnosis, we can strive towards the WHO’s vision of eliminating cervical cancer as a public health problem on a global scale.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8989294/
- https://link.springer.com/article/10.1007/s40944-021-00602-z
- https://hpvcentre.net/statistics/reports/IND_FS.pdf
- https://www.cdc.gov/vaccines/vpd/hpv/public/index.html
- https://www.who.int/news-room/fact-sheets/detail/human-papilloma-virus-and-cancer#:~:text=Condoms%20help%20prevent%20HPV%20but,go%20on%20to%20become%20cancer.
- https://www.who.int/initiatives/cervical-cancer-elimination-initiative#:~:text=Each%20country%20should%20meet%20the,cancer%20within%20the%20next%20century.
- Cervical Cancer Screening – NCI